Minus the City: What You Need to Know About the O-Shot
In last week’s Minus the City, I mentioned how Dr. Jennifer Lincoln spoke on the phenomenon of the O-shot. Before then, I had no idea this was an actual medical procedure, and I’m sure that I wasn’t alone in this. So let’s talk about whether the procedure is a miracle vaginal healer or indicative of the failures of sex-ed.
As some might already know, the O-shot procedure involves the injection of plasma rich platelets, or PRP, taken from your own blood, into the clitoris, the clitoral hood and inside the vagina, into the vaginal walls. The procedure is said to increase overall arousal in that area, making it easier for women to orgasm both through clitoral stimulation and vaginal penetration.
The same concept–using your blood as medicine–is a popular trend. Kim Kardashian’s blood facial, or the “Vampire Facial,” involves the injection of your own blood into your face, which is said to rejuvenate the skin. PRP therapy is also used by athletes for its healing properties, allowing them to quickly recover from various injuries. In these cases, PRP displays restorative results, but is the inability to orgasm vaginally something that needs to be restored? Can a vagina really be broken in need of healing?
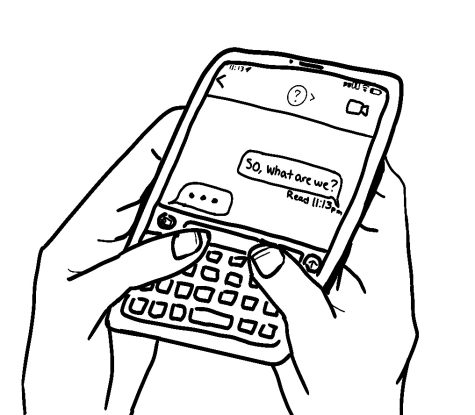
The use of PRP to improve sexual satisfaction was initiated by Dr. Charles Runels, who says the idea struck him after an encounter with a “beautiful, tall” patient who explained having a tough time achieving any sort of arousal. Dr. Runels told his patient about the idea and she allowed him to perform the procedure on her. That night he received a text from her saying she was absolutely dumbfounded by the results, having orgasmed within a couple of minutes of using a vibrator on medium speed. He was completely elated and surprised that her results were so quick, given this type of therapy usually takes 8 weeks to “do its job”, while her results took a couple of hours.
Runels claims the O-shot is backed by medical science, although there is no peer-reviewed literature on the use of PRP to “bring back” orgasms in women. Runels says there have been studies done to support it; there are a total of three studies done, one of which was only done on 3 women, which does not even seem like a legitimate study. And still, these studies focus on the effect of PRP on inflammation due to vaginal mesh, not on orgasms. The one study conducted by Runels himself involves 11 women with different diagnoses, 64% of which noted some form of improvement. Dr. Jen Gunter, another OB/GYN committed to debunking sexual myths, explained her amusement at the fact that Runels renamed his office as “Medical School” in this paper, and not to mention, misspelled the word dyspareunia several times.
If you do your research, all the signs scream “don’t do it.” But one can’t help but wonder, “then why does it exist? Why is it so popular and why do women continue to have the procedure?” Professor of Sociology and Women’s Studies Meika Loe says it all points to the failure of sex-ed curricula.
“Since we don’t have comprehensive sex-ed, profit-making ventures like the O-Shot do this work for a pretty penny, once again turning women into medical guinea pigs,” she said. “I find this to be a troubling reality. It reinforces our medical quick-fix culture, raises gendered insecurities, exploits sexual consumerism and doesn’t help us make progress structurally when it comes to major gaps in sex education.”